ARMHS Top-Level Documentation Overview
28.04.2005
ARMHS, Support Posts
This is an example timeline and related requirements for ARMHS Documentation in BreezyNotes:
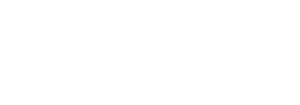
- ARMHS Diagnostic Assessment (Valid if eSigned by provider)
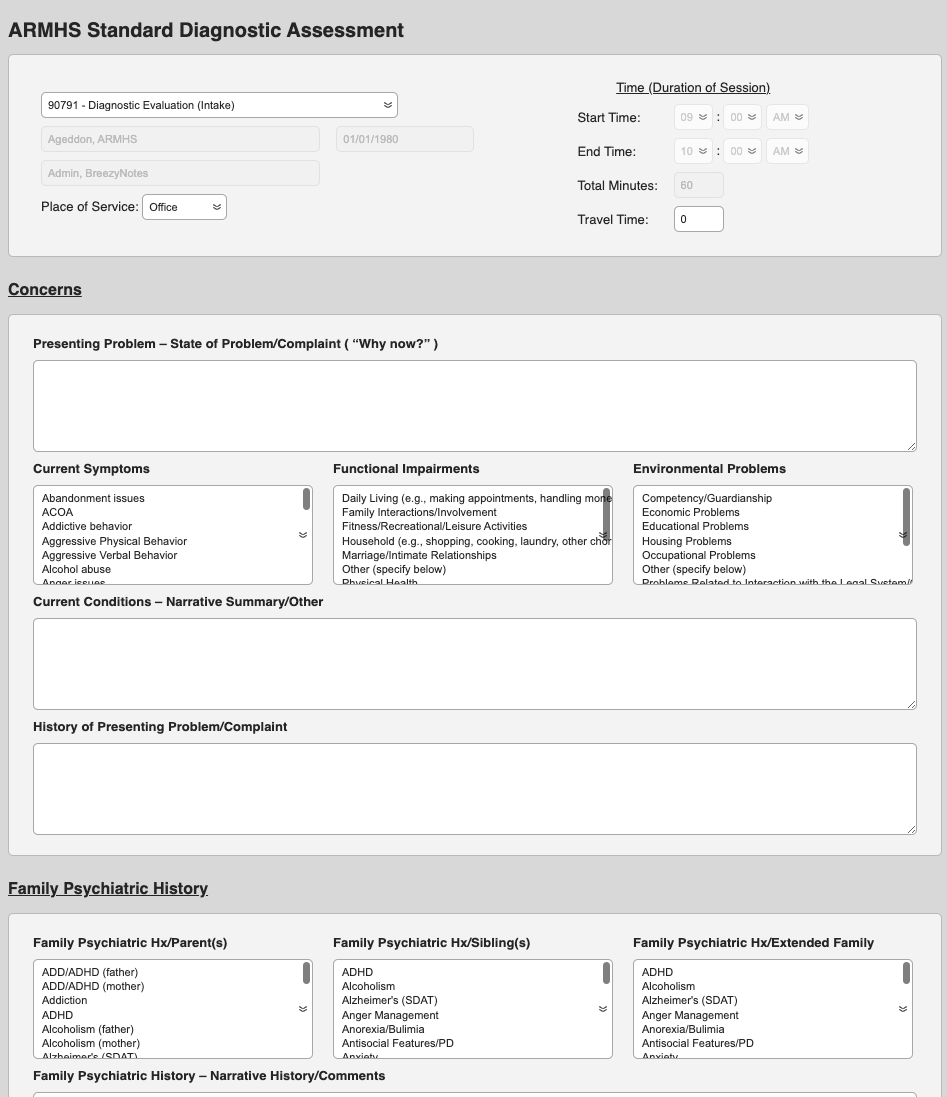
- ARMHS Functional Assessment (Valid if eSigned by provider)
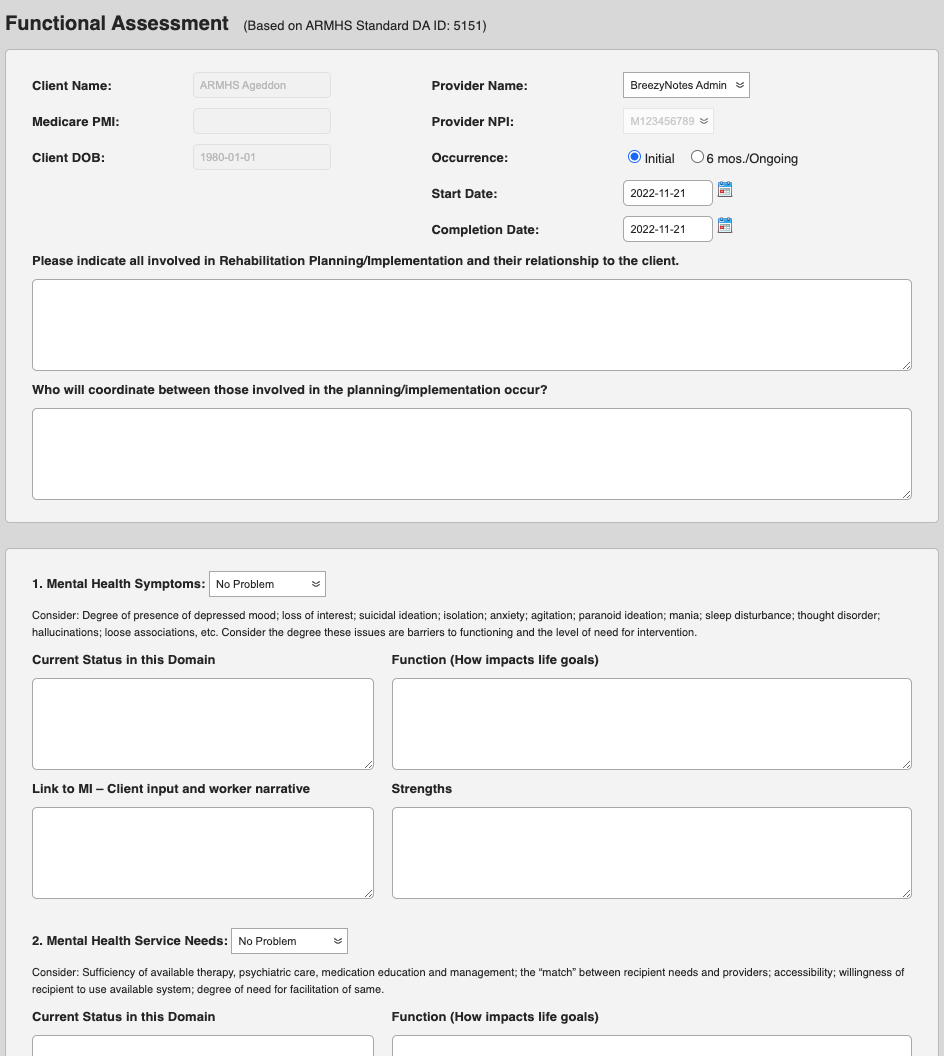
- Complete ARMHS Progress Note – FA for any time(s) any work the FA is done.
- Complete ARMHS Progress Note – FA for any time(s) any work the FA is done.
- ARMHS Individual Treatment Plan
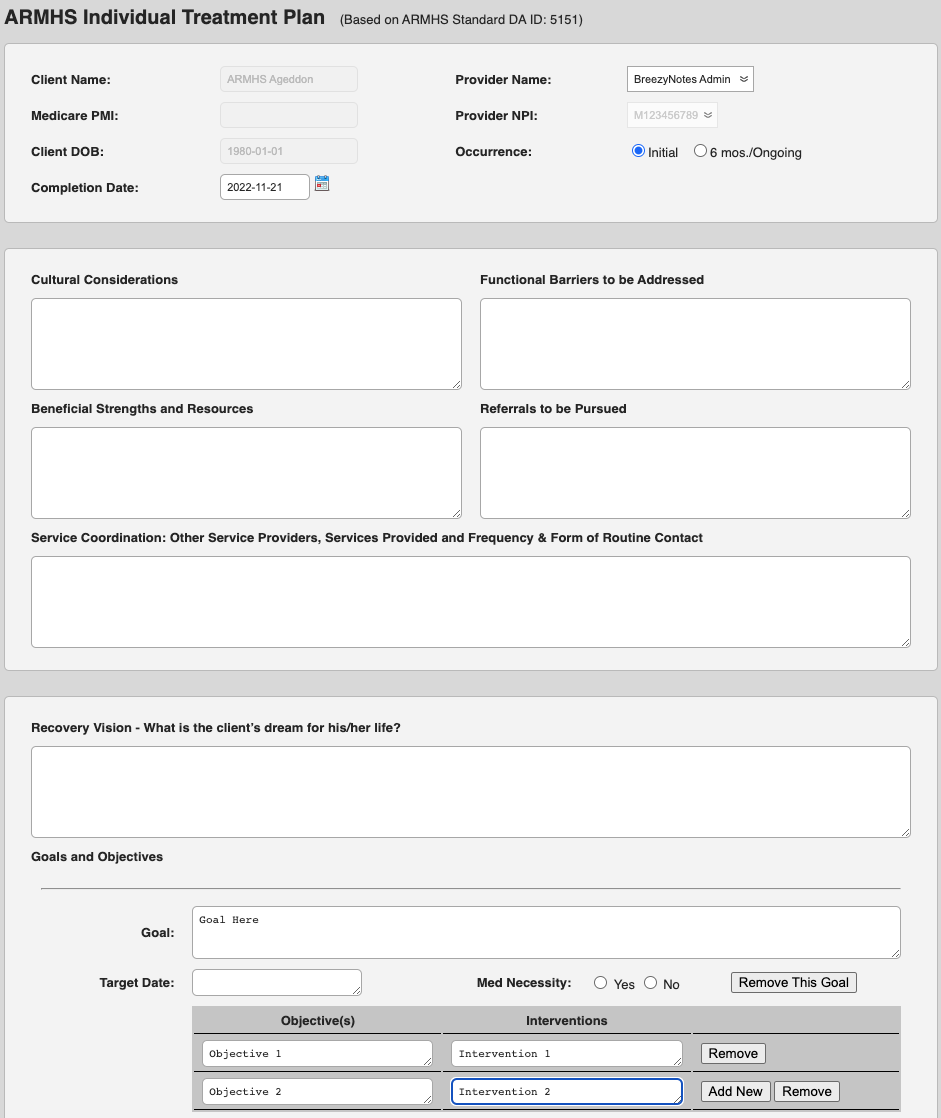
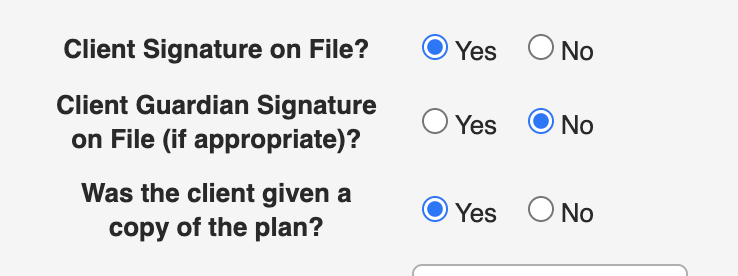 (Valid if 1. eSigned by provider and 2. Client or Guardian Signature set to “Yes”):
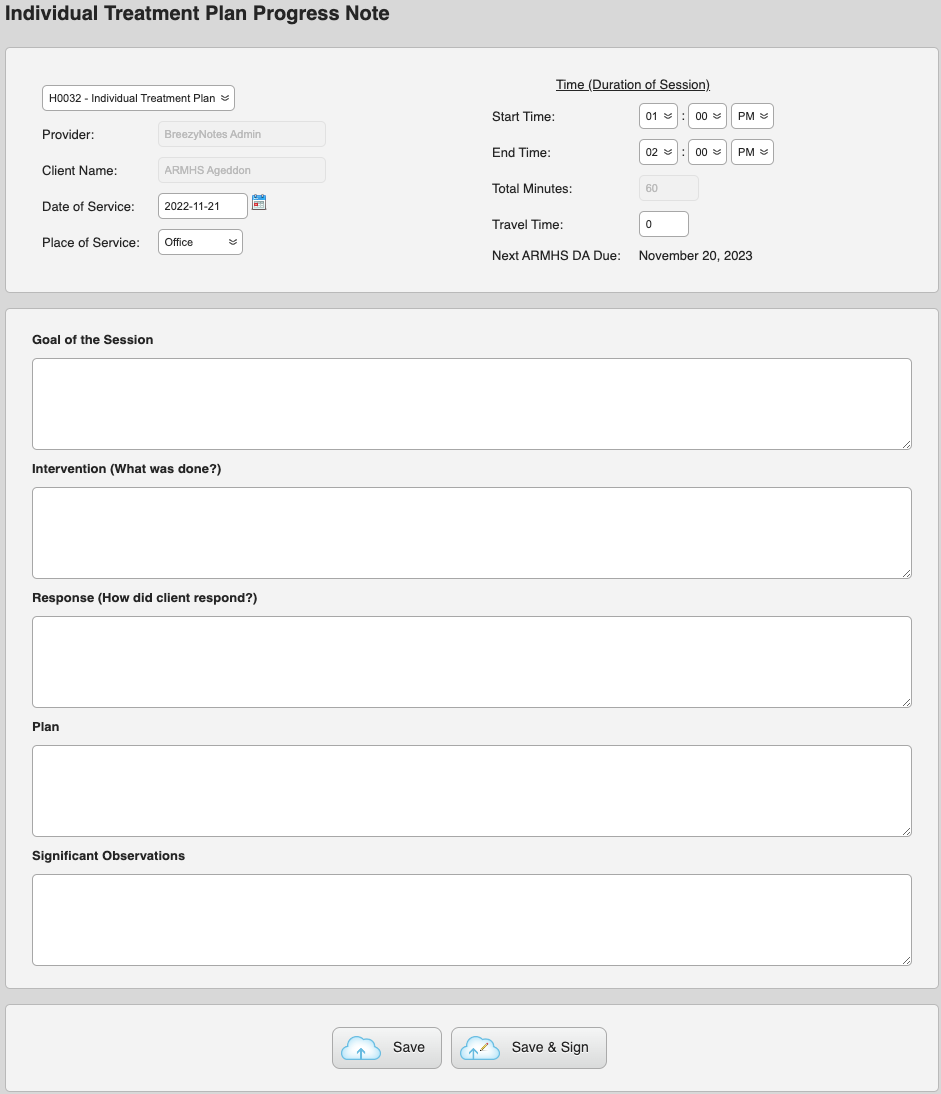
(Valid if 1. eSigned by provider and 2. Client or Guardian Signature set to “Yes”): - Complete ARMHS Progress Note – ITP for any time(s) work on ITP is done.
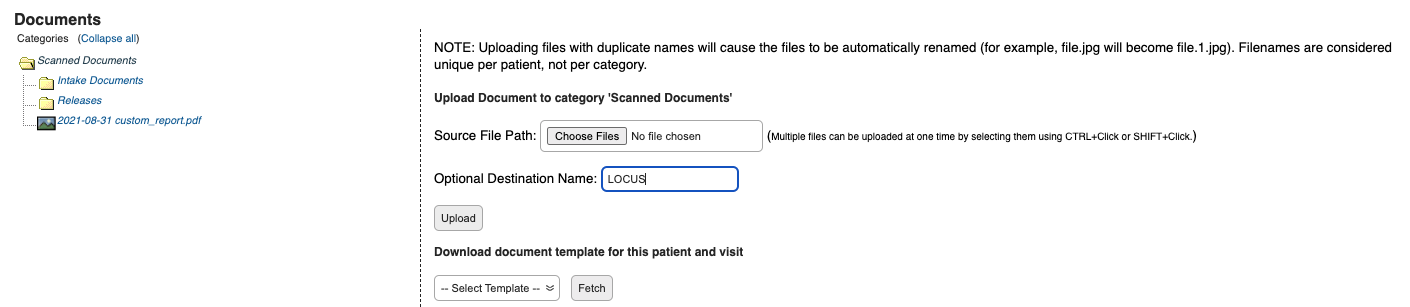
- Complete LOCUS and upload to client’s Scan Documents (if applicable)
- Start doing ARMHS Progress Note – BLS
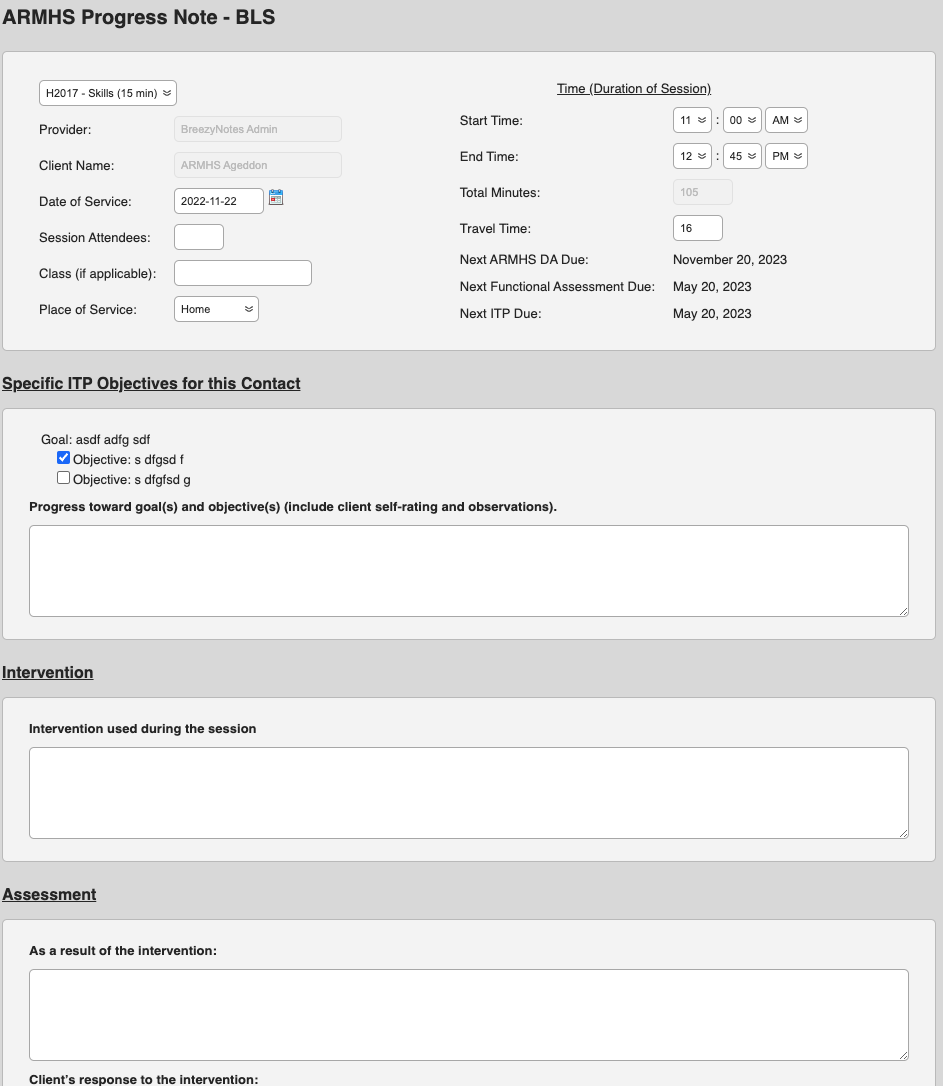
This can only be done if:
- DA is signed and is less than 365 Days old based on DOS
- FA is signed and is less than 180 Days old
- ITP is signed, Client or Guardian Signature is “Yes,” and is less than 180 Days old.
If one of the above is not done, or is nearing a due date, there will be a notification in the ARMHS Progress Note – BLS:
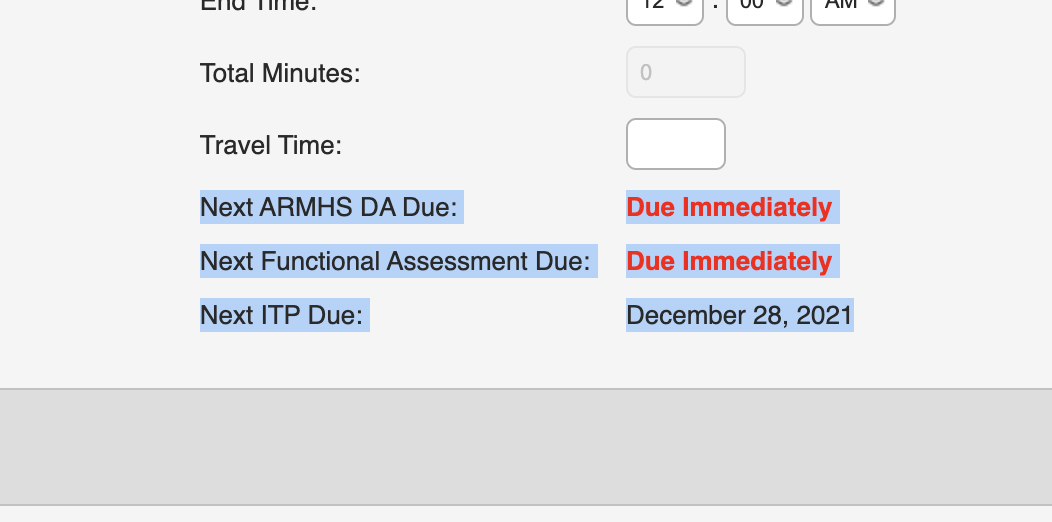
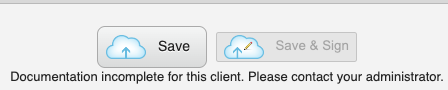
MHPs CAN NOT Save and Sign the form and there is an alert that documentation is incomplete:
Any other forms not in our system can be completed outside and uploaded to the client’s Scan Documents folder, which we can customize to fit your needs.
ARMHS And Outpatient Behavioral Health
If you are doing ARMHS and Outpatient Mental Health, make sure to use the ARMHS Standard Diagnostic Assessment and not the Diagnostic Assessment.
Also make sure you use the ARMHS Individual Treatment Plan and not the Individual Treatment Plan.