Review Submitted Claims
When you click Save, Sign & Submit or Submit to Clearinghouse claims are queued to be sent to the clearinghouse every 15 minutes. Within a few minutes of receiving a claims file (.837), ABILITY will process and validate the claims before sending them on to the insurance company.
To review these claims, click on the Professional Claims tile or choose “Professional” from the Claims menu.
 or
or 
You will then see a table of all your claims submitted based on your settings in the Profiler:
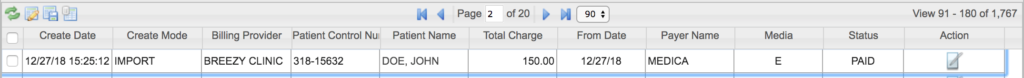
You can (and should!) log in to review your submitted claims on a regular basis. Doing so allows you to track the status of the claim from the moment it was received to payment.
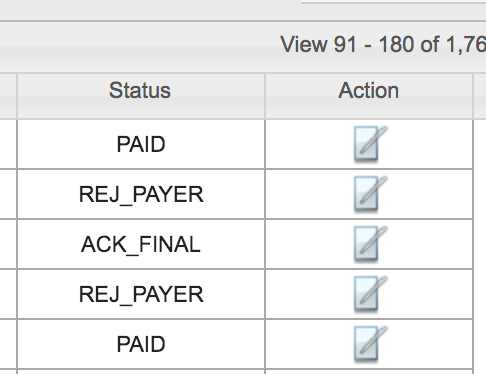
There are 21 Status categories, but the most common are:
- VALIDATED – Ability received and validated the claim
- ERROR – Ability received the claim, but there was an error (Learn to fix it here)
- ACK_PENDING – Ability sent the claim to the payer and is waiting for acknowledgement
- ACK_FINAL – Ability received acknowledgement that the payer received the claim
- REJ_PAYER – The payer rejected the claim (Learn to fix it here)
- DENIED – The payer denied the claim (Learn to fix it here)
- PAID – The payer paid the claim (Ability received a remit)
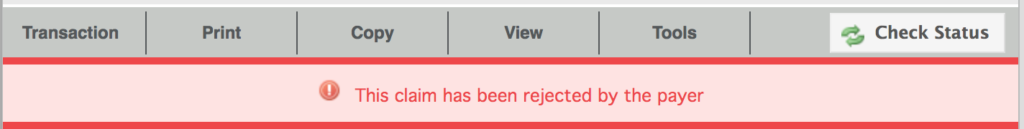
To learn more about the Status of a claim or to see claim details, click the Action icon (![]() ). At the top of the Overview, you’ll see a menu and a claim status notification:
). At the top of the Overview, you’ll see a menu and a claim status notification:
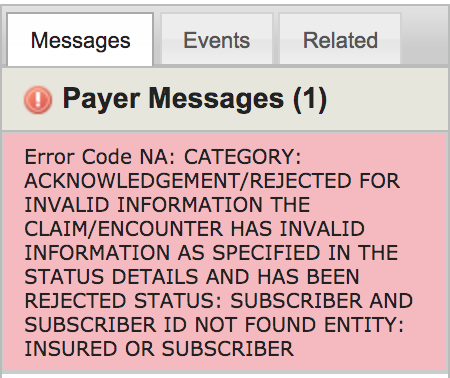
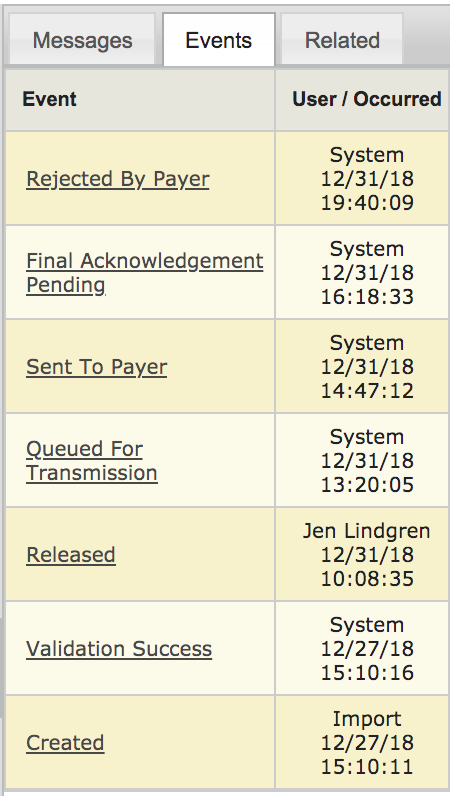
To the right is a message center that will further explain the claim status and give you the option to see all events related to this claim:
For details on Fixing a Claim, click here.