(Ver. 3.0) – ARMHS Top-Level Documentation Overview
This is an example timeline and related requirements for ARMHS Documentation in BreezyNotes. These forms can be accessed through the calendar, the client’s chart, or both.
Opening a form through the calendar:
Drag the client’s name to the calendar and an appointment window pops up:
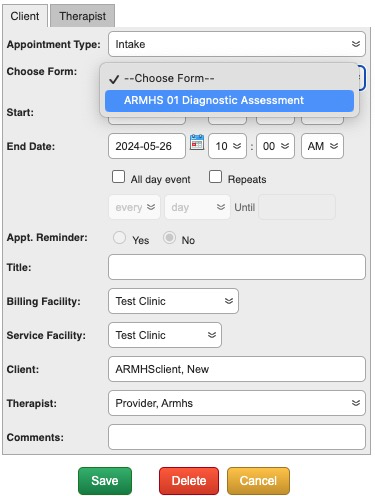
Choose the Appointment Type and Form, check Facility, Client, and Therapist details and click “Save”. An appointment box is added to the calendar:

When it’s time to check in the client and start your note, click the notepad icon on the appointment:
![]()
This will open your form.
IMPORTANT NOTE: Not all forms are available via the calendar. Typically we keep non-billable forms, like the Functional Assessment and Individual Treatment plan forms in the Forms dropdown of the client’s chart. This is because these forms are billed using Progress Notes.
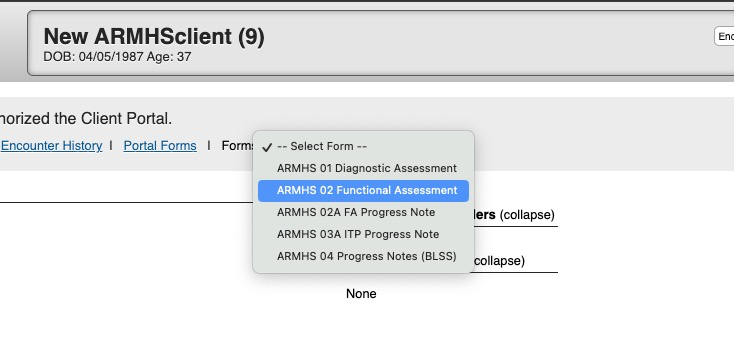
Opening a Form via the Client’s chart:
Click on the a client’s name to open their chart.
In the Forms dropdown, choose the form you’d like to open:
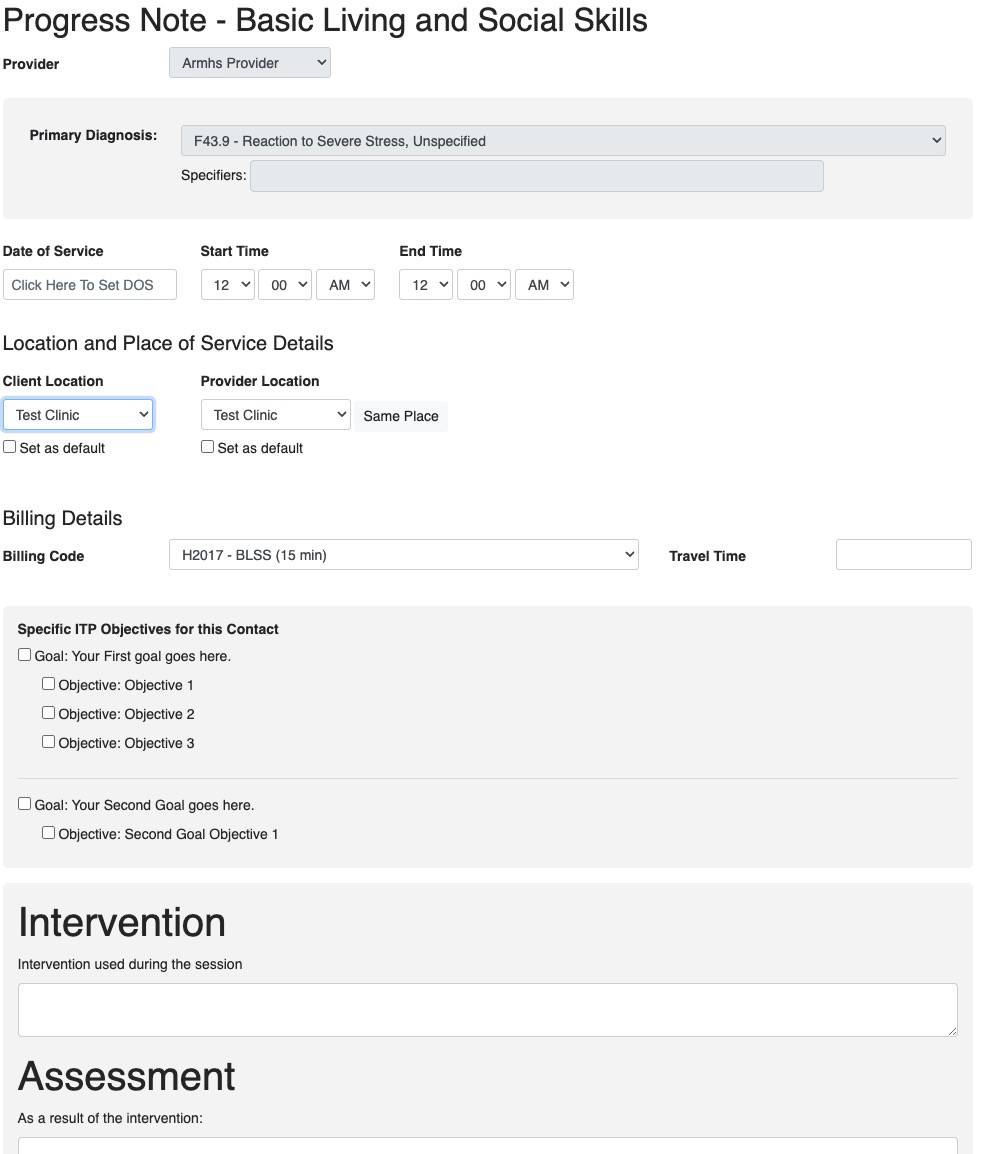
You will be brought to that form where you will need to manually enter the DOS and Start/End Time before starting on the form.
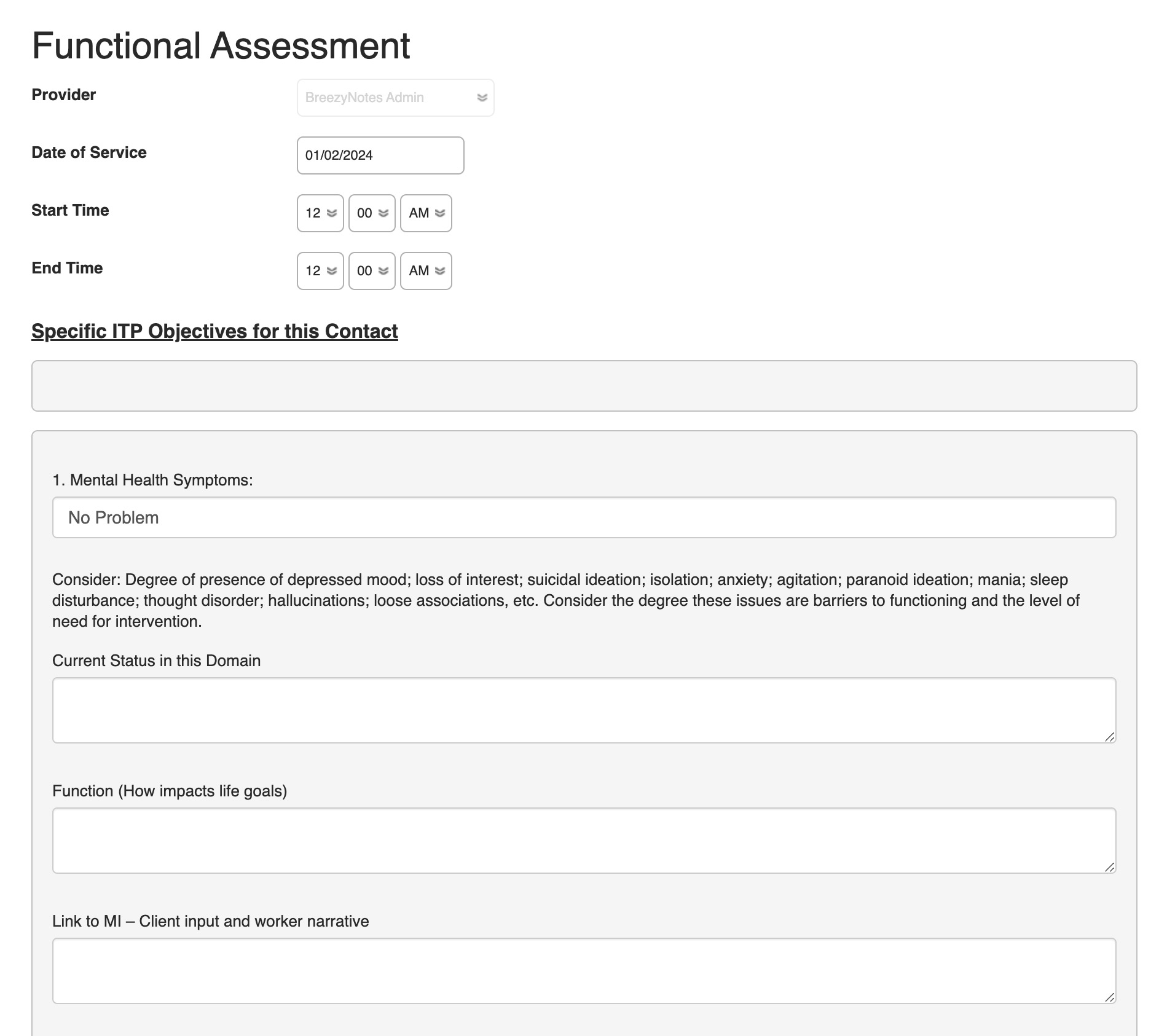
Complete the form and click Save & Sign.
IMPORTANT NOTE: Not all forms are available via the client chart.
ARMHS Documentation Forms in Order of Completion
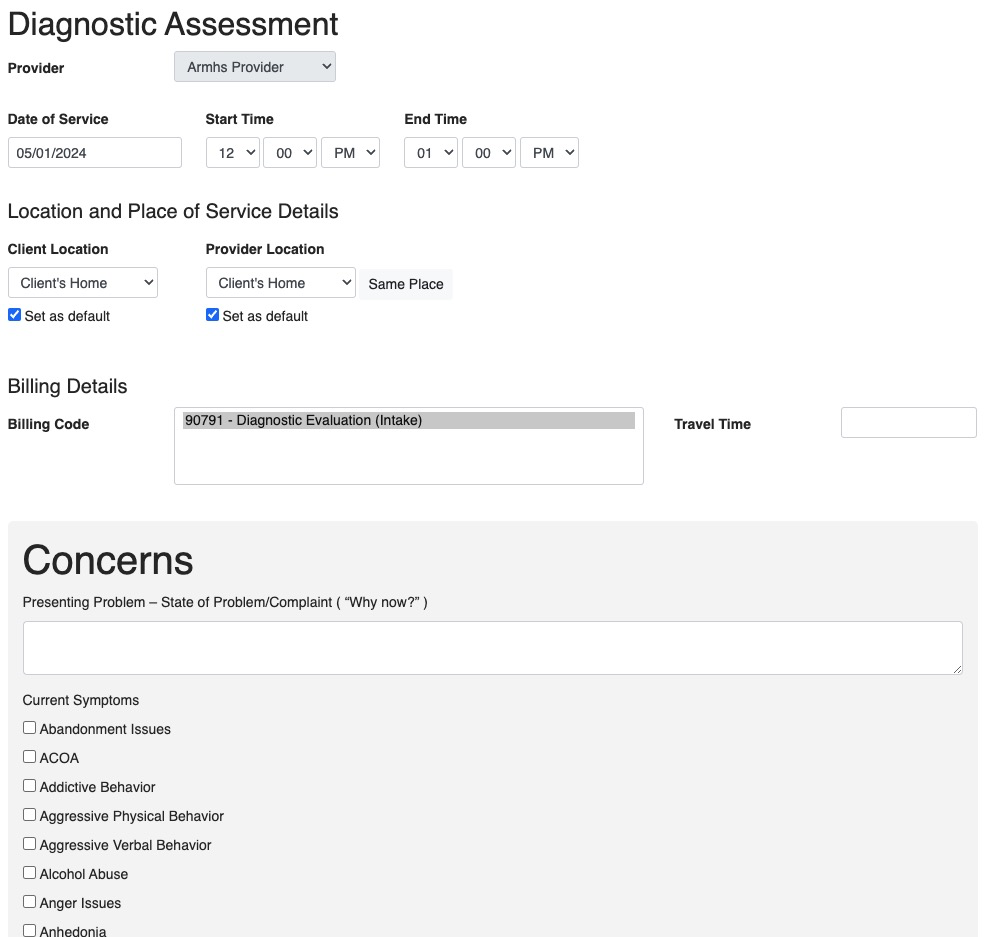
ARMHS 01 Diagnostic Assessment
- Valid only when signed by a licensed provider or clinical trainee
- Not available for MHPs to see
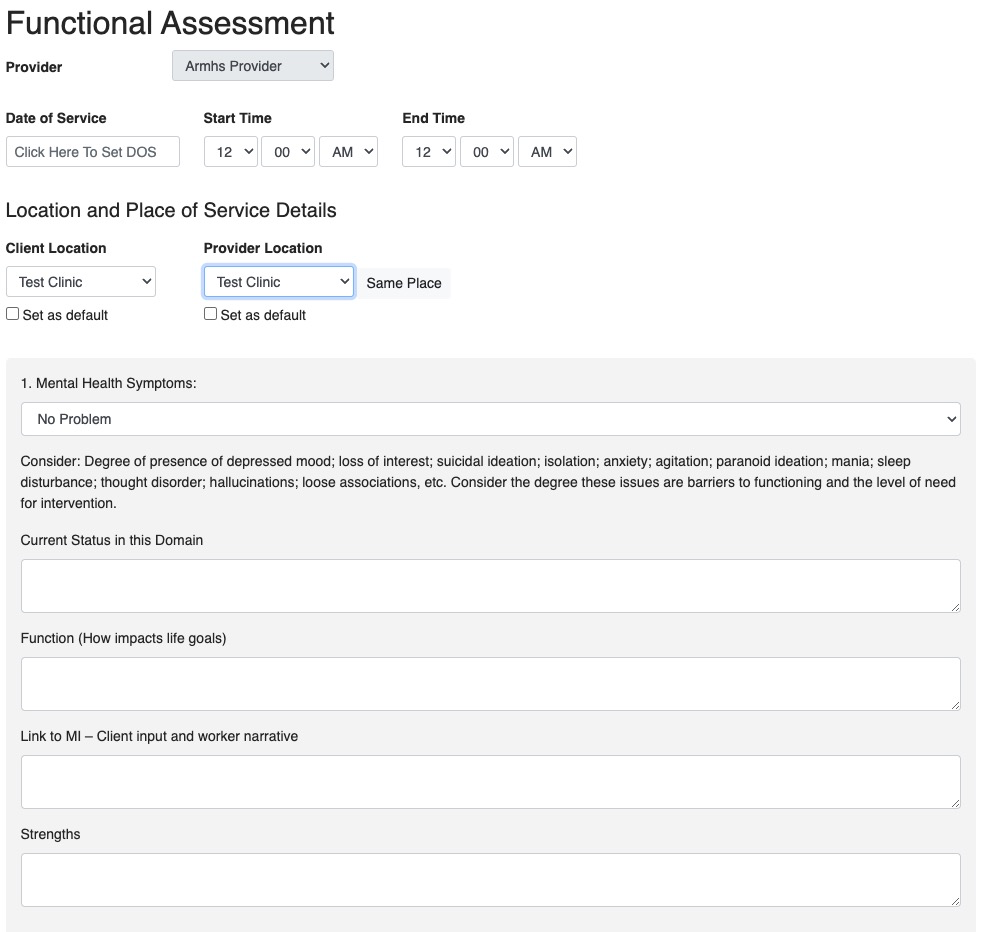
ARMHS 02 Functional Assessment
- Valid only if signed by a licensed provider, trainee or practitioner with sufficient rights to see the form.
- Some MHPs may not have access to the Functional Assessment.
- Time spent on this form is billed with the ARMHS 02A FA Progress Note.
- When you Save & Close or Save & Sign this note, it will ask if you want to complete the ARMHS 02A FA Progress Note.
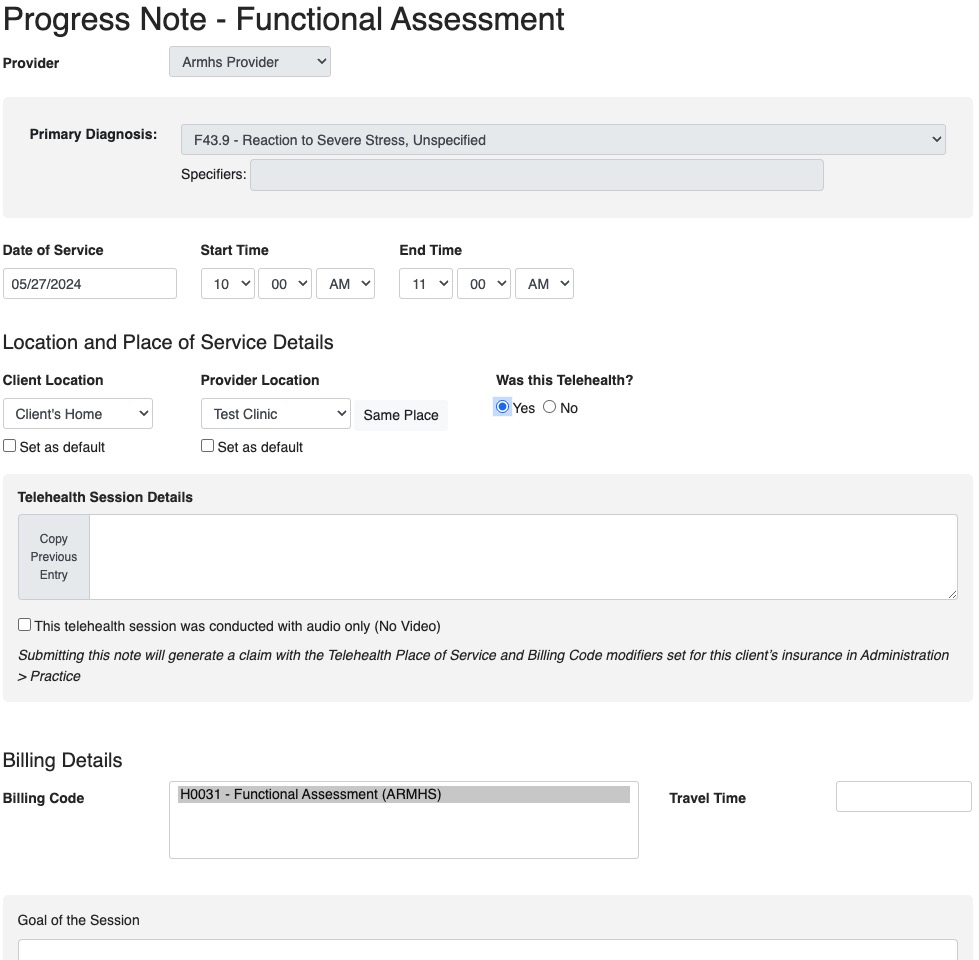
ARMHS 02A FA Progress Note
- Use this note to bill for time spent on the Functional Assessment.
- One session may be billed per day that it is worked on.
- No more than six sessions per calendar year, which means up to three sessions per each 180 day time period
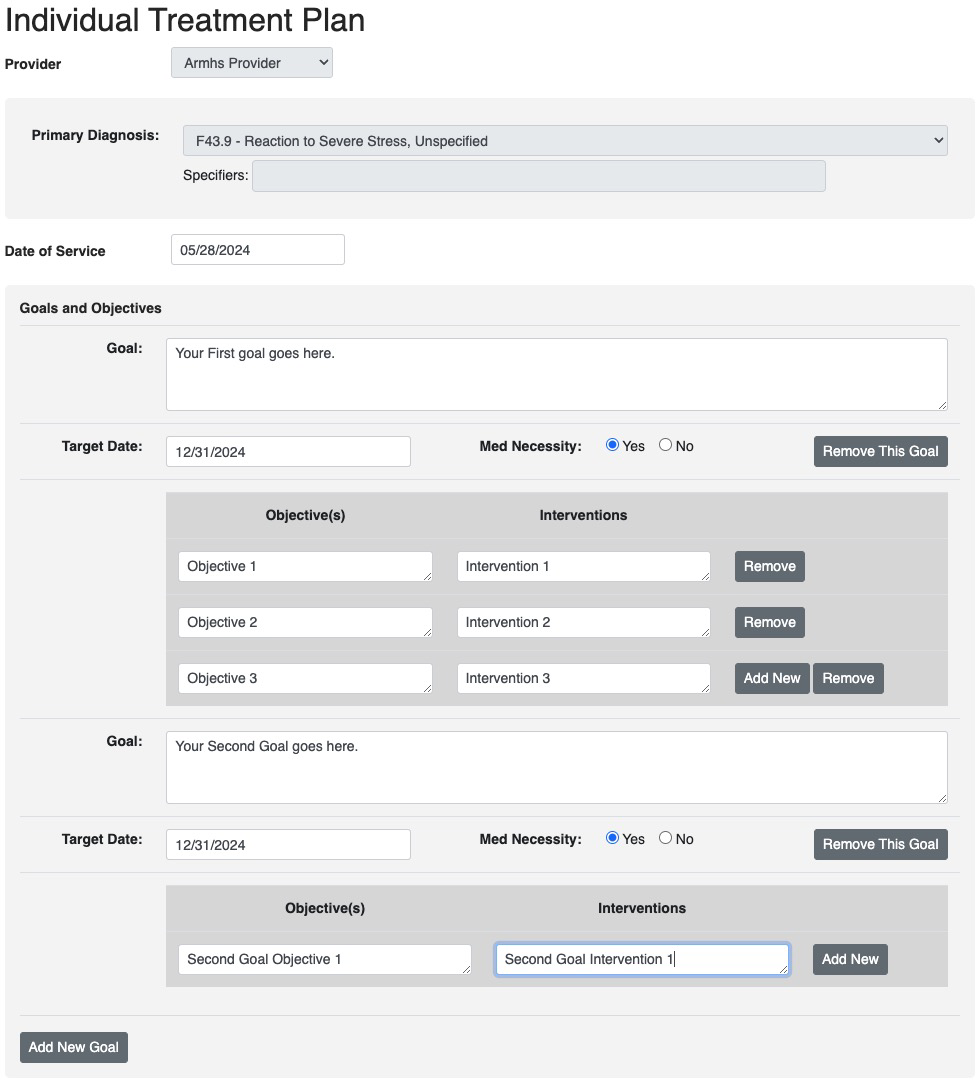
ARMHS 03 Individual Treatment Plan
- Must be signed by the provider AND
- The field Is the Client or Guardian Signature on File? must be set to “Yes”
- Some MHPs may not have access to the Individual Treatment Plan.
- Time spent on this form is billed with the ARMHS 03A ITP Progress Note.
- When you Save & Close or Save & Sign this note, it will ask if you want to complete the ARMHS 03A ITP Progress Note.
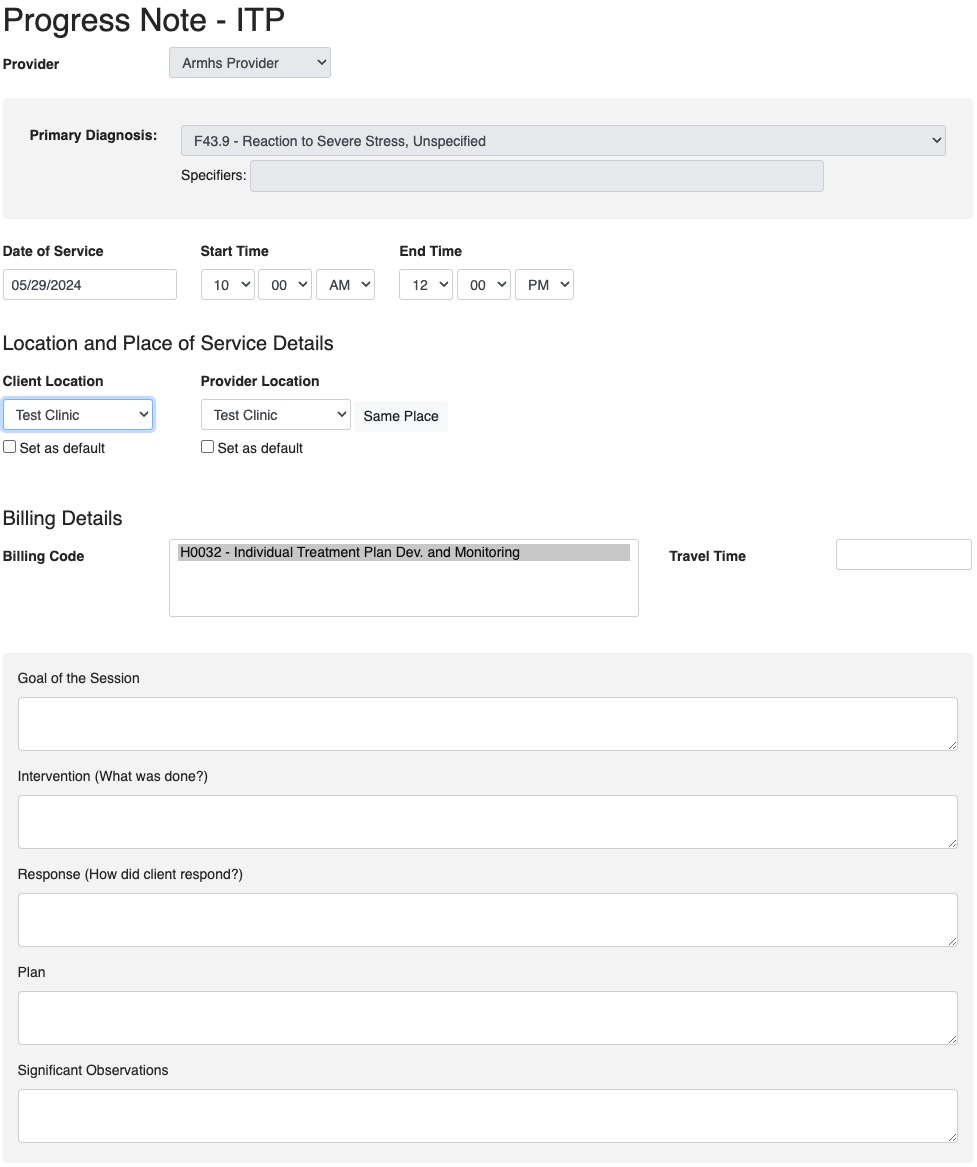
ARMHS 03A ITP Progress Note
- Use this note to bill for time spent on the Individual Treatment Plan.
- One session may be billed per day that it is worked on.
- No more than four sessions per calendar year, which means up to two sessions per each 180 day time period
ARMHS 04 Progress Note (BLSS)
- In order to complete this note the Diagnostic Assessment, Functional Assessment and Individual Treatment Plan must all be valid
- Diagnostic Assessment must be less than one year old and be signed by a clinician or clinical trainee.
- Functional Assessment must be less than 180 days old and be signed by a clinician, clinical trainee or MHP.
- Individual Treatment Plan must be less than 180 days old, indicate a client or guardian signature is on file, and be signed by a clinician, clinical trainee or MHP.